Adhering to Scottish standards of care following a hip fracture improves the survival of patients.
Adhering to Scottish standards of care following a hip fracture not only improves the survival of patients, but also reduces the duration of hospital admission and reduces the need for transfer to high-care settings, according to a new study.
Andrew Hall and Luke Farrow who led the study at The University of Aberdeen state that Scotland ‘is leading the way in the care of hip fracture patients, and the standards set up and down the country are a benchmark to which other nations can aspire’.
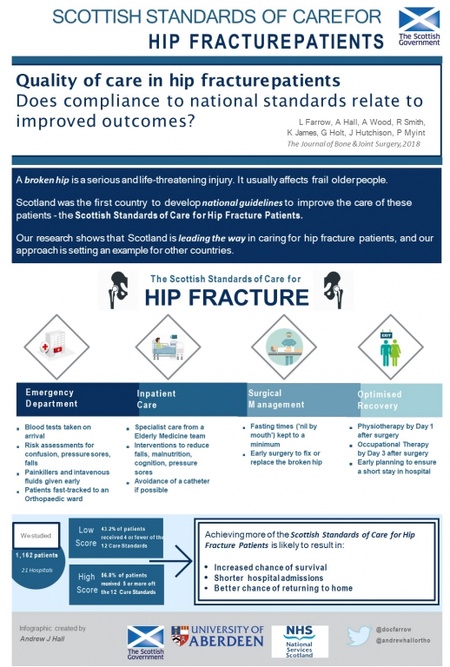
They examined data from over 1,100 patients from 21 different hospitals across Scotland. A total of 1,162 patients aged over 50 years and admitted with a hip fracture were included in the study to find if Scottish standards of care (Scottish Standards of Care for Hip Fracture Patients (SSCHFP)) provided tangible benefits to patients.
Published this week in The Journal of Bone & Joint Surgery, the study concluded that adherence to standards was related to several positive outcomes, including reducing the chance of death, reducing the amount of time spent in hospital post-surgery, and reducing the need for complex aftercare.
Scotland was the first country in the world to introduce the care standards for this type of injury.
Luke Farrow explains: “By implementing the Scottish Standards of Care for Hip Fracture Patients (SSCHFP), Scotland became the first country to have a nationally-agreed, evidence-based collection of care standards to ensure a consistently high level of care in this setting. Despite implementation of the SSCHFP in 2014, there was previously no information assessing the impact of such standards on patient outcomes. This was the aim of our study - to find if these standards are succeeding in what they set out to achieve.
“Optimising the perioperative care of patients with a hip fracture is a key healthcare priority, particularly with an ageing population and a significant predicted rise in the number of individuals suffering a hip fracture by 2030. The risk of death at one year after such an injury is currently up to 30%; much higher than more commonly recognised health problems such as heart attacks and strokes.”
There is a raft of standards within the SSCHFP, which were summarised into twelve standards and were included in the study. These standards range from fasting after surgery to time to access physiotherapy, and they are designed to help promote better care and a faster recovery.
Luke Farrow adds: “In the first review of these standards, we found clear evidence that adherence to the SSCHFP is associated with better patient outcomes. These findings confirm the clinical utility of the SSCHFP and support their use as a benchmarking tool to improve quality of care in hip fracture.
“We would hope that this study will encourage healthcare professionals to adhere to the SSCHFP and also inform the conception of further standards in the future.”
Andrew Hall, Honorary Research Fellow at The University, who co-authored the study said: “The evidence from this study serves as an incentive for hospitals to continue to seek improvements in how they treat patients with hip fracture. The Scottish Hip Fracture Audit has already set in motion measures which will ensure that more patients receive the best possible care.
“We believe that the success of the Scottish Standards means that Scotland is leading the way in the care of hip fracture patients, and the standards set up and down the country are a benchmark to which other nations can aspire.”
Graeme Holt, a Consultant Orthopaedic Surgeon and Chair of the Hip Fracture Steering Group, added: “Hip fracture injury is set to increase in number by approximately 50% in the next 17 years as a result of changes in population demographics. Given the common nature of this injury and the cost associated with managing hip fracture, it is essential that we deliver high quality, effective and efficient care to this vulnerable patient group.
“Since the introduction of the Scottish Hip Fracture Audit and quality improvement pathway, we have observed significant improvement across all indicators, in particular the delivery of care of the elderly medical interventions, more patients being discharged from hospital by 30 days following injury, a reduced length of average hospital stay, reduced mortality, and significant cost efficiencies.
“Whilst we acknowledge that significant progress has been made, further work is required and we will continue to work towards delivering sustainable improvement which benefits all patients who sustain hip and other fragility fractures.”
ENDS