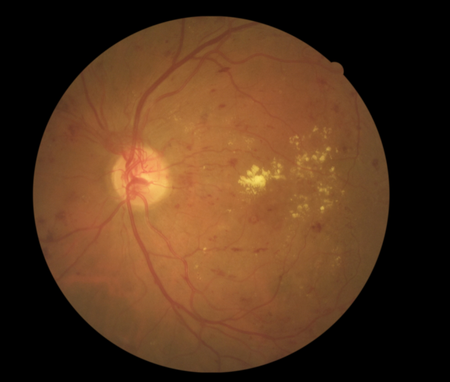
Diabetic retinopathy - a common complication of diabetes which occurs when high blood sugar levels damage the cells at the back of the eye - is the biggest cause of blindness in the working population globally.
It is treatable if detected early but standards of screening vary vastly around the world. Researchers from the University of Aberdeen and NHS Grampian are exporting Scottish expertise in the field to Africa, where diabetes is a growing problem, with the aim of improving international standards.
In 2007, Scotland became the first country to introduce a rigorous online testing programme for those who screen for diabetic retinopathy. It requires every screener to undertake a bi-annual online review to test the accuracy of their diagnoses.
But in many developing countries, where health services are private, those conducting the photo screening have often completed only limited training.
The Aberdeen team, made up of Drs Roger Staff and John Olson, was asked to investigate the issue by the Ophthalmological Society of South Africa. Their study, published in the South African Medical Journal, found many weaknesses in the screener’s performance which could result in the condition going undetected.
Dr Staff said: “There is a real lack of standardisation in the training of screeners in South Africa and performance varied significantly when we compared their performance to a group of expert Scottish screeners. Those who we tested had come forward voluntarily so we suspect that there are probably many more deficiencies in the screening process that we were not able to measure.
“However, a small amount of training could lead to significant health gains. To provide the impetus for this to happen, we first needed to demonstrate that there was a problem and our study highlights a number of issues which need to be addressed urgently.
“Diabetic retinopathy is a growing problem in sub-Saharan Africa, where the prevalence of diabetes is predicted to triple by 2020 from levels in 2000.”
“Diabetic eye disease is the single biggest cause of blindness in the working population but is easily preventable. It is clear that effective interventions are required in the near-future to avert the anticipated health burden.”
The Aberdeen team will now work with the Ophthalmological Society of South Africa to devise training programmes which they hope could eventually be rolled out worldwide.
Dr Staff added: “Following on from our report, we will share ideas for how the system in South Africa can be improved.
“The online model developed in Scotland could provide the basis for enhancements to the training procedure around the world.
“By using the internet, we can make it easily accessible to all and we believe there are cheap, and easily implementable, options which could reduce the risk of blindness for those with diabetic retinopathy who do not have access to the advanced healthcare enjoyed in developed countries.
“We will now be working to develop a detailed programme to improve standards first in South Africa, with a view to enhancing practice in developing countries.”
The full report ‘Quality assurance in diabetic retinal screening in South Africa’can be viewed online at http://www.samj.org.za/index.php/samj/article/view/8678/6196
ENDS
Note to editors:
Dr Stephen Cook from The Ophthalmological Society of South Africa & Walter Sisulu University, Mthatha, South Africa gave the following testimonial for the project:
“The University of Aberdeen External Quality Assurance software and support system facilitate the development of learning, critical to the implementation of a diabetic retinopathy screening system in South Africa and is a cornerstone of the SA DR screening programme.”