Corticosteroids
- Beclometasone
- Budesonide
- Fluticasone
- Prednisolone
- Dexamethasone
- Regular prevention of asthma
- Maintenance therapy in COPD in combination with long acting bronchodilator if FEV1 <50% (note that some patients with COPD do not have steroid reversibility)
- Hayfever (intra-nasal use)
- Treatment of acute exacerbation of asthma
- Long term low dose maintenance therapy in asthma
- Treatment of acute exacerbation of COPD (COPD Guidance)
- Long term low dose maintenance therapy in COPD (rarely indicated)
- Bronchospasm or partial obstruction
- Dyspnoea in palliation
- Pregnancy
- Breast feeding (inhaled corticosteroid unlikely to be significantly present in breast milk)
Corticosteroids have an anti-inflammatory effect in many tissues. Virtually all cells contain steroid receptors which then bind to DNA to prevent or induce gene expression.
In the context of inflammation, corticosteroids:
- Decrease neutrophil and macrophage recruitment and action
- Decrease fibroblast formation
- Decrease osteoblast and increase osteoclast activity
- Decrease production of prostanoids
- Decrease production of cytokines
- Decrease histamine release
- Decrease IgG production
- Aerosol: Taken as required, via an MDI (metered dose inhaler) or a dry powder device +/- a spacer device. Note: there are a number of dry powder formulations available.
- Intranasal
- Oral
- Intravenous (severe exacerbations only)
- The MHRA has recommended that beclomethasone dipropionate inhalers (Qvar, Clenil Modulite) be prescribed by brand as they are not interchangeable with other beclomethasone based inhalers.
There are a wide range of adverse effects, which are associated with systemic absorption. These include:
- Osteoporosis
- Ischaemic necrosis of femoral head
- Cataract
- Acute Glaucoma
- Cushingoid features including weight gain
- Increased susceptibility to infection, particularly TB, varicella and candida
- Hyperglycaemia potentially leading to type 2 diabetes mellitus.
- Hypertension
- Fluid retention and worsening of heart failure
- Hypokalaemia
- Mask inflammatory response
- Mental disturbance including psychosis
- Addisonian crisis in abrupt withdrawal
Pharmacodynamic interactions can occur where steroid effects increase or antagonise the effect of other drugs. For example:
- Steroids can mask the adverse effects of NSAIDs.
- Hypokalaemia can be made worse if steroids are used in combination with other drugs which lower potassium.
- Antihypertensive and hypoglycaemic agents are antagonised by corticosteroids.
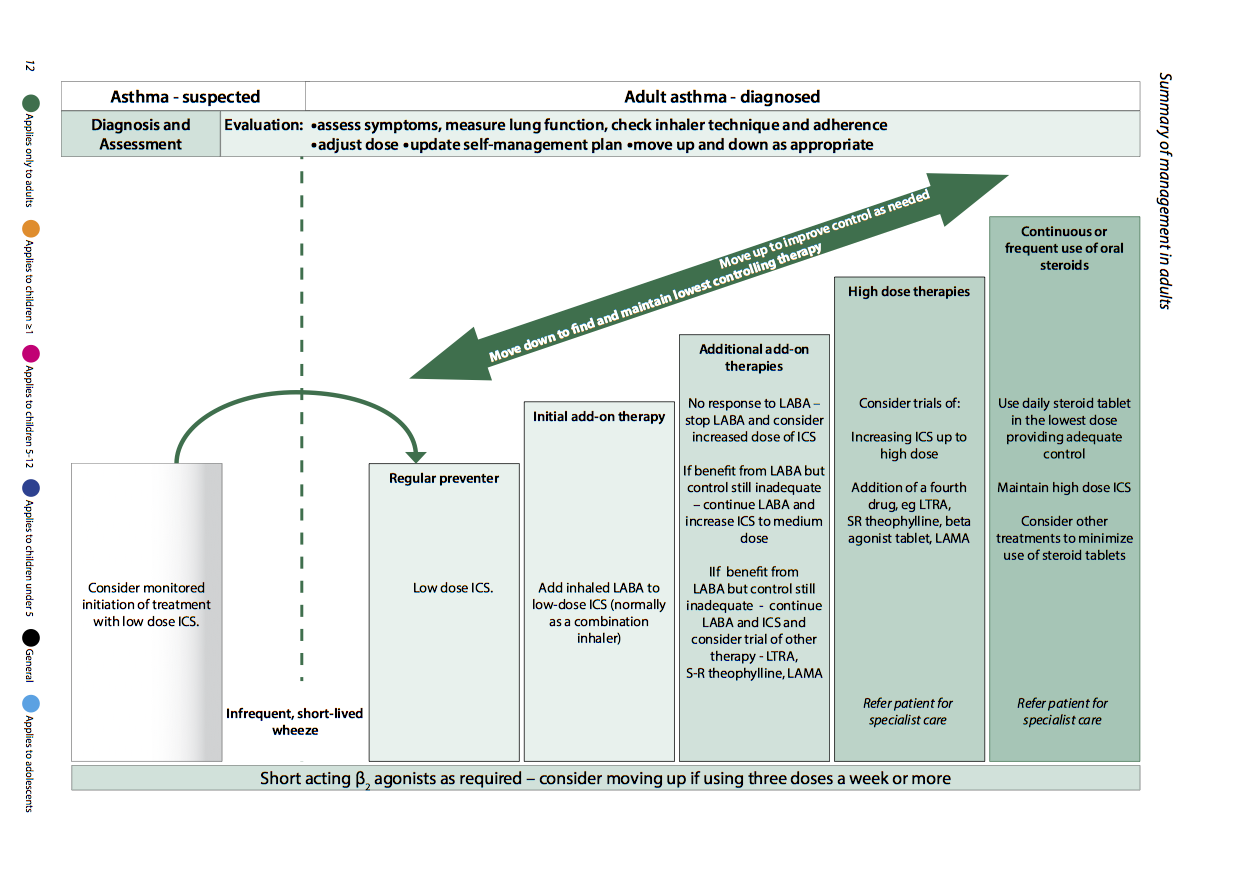
Many asthmatic patents receive dual therapy with corticosteroids and β2 agonists. Ensure the patient understands that short acting β2 agonists only relieve the symptoms of asthma, patients often referred to this as a 'reliever'. In comparison corticosteroids are referred to as a 'preventer'. To achieve maximum efficacy, it is important to stress the different roles these drugs play in the treatment of asthma.
Patients should be informed that it can take several days for inhaled corticosteroids to take effect and so, they should continue taking them even if there is no immediate difference in symptoms within the first few days.
Inhaled corticosteroids need to be taken regularly to gain maximum benefit, therefore patient compliance is very important.
Whilst side effects with inhaled corticosteroids are uncommon, some patients may be at an increased risk of oral thrush. Therefore, it is recommended that patients rinse their mouths with water after taking their inhaled corticosteroids.
Ensure that the patent knows how to use an inhaler device (+/- spacer) correctly. Ask them to demonstrate how to use it.
Patients prescribed long term corticosteroids should be provided with a "steroid card" (pictured) and warned not to stop their medication suddenly. In instances where corticosteroids are used for more than 3 weeks, or in multiple short courses, or at very high doses, patients should be given a reducing regime.
Oral steroids are best taken in the morning to match the body's normal diurnal variation.
All patents with asthma require an annual asthma review, with either a doctor or asthma nurse specialist.