Neuromuscular Blocking Drugs
Examples
Non-depolarising neuromuscular blocking drugs
- Atracurium
- Mivacurium
- Rocuronium
- Suxamethonium
Indications
When generalised muscle relaxation is required in addition to general anaesthesia.
Contraindications
Non-depolarising neuromuscular blocking drugs
Contraindications
- Allergy
- Neuromuscular disease or dysfunction
- Hepatorenal impairment (prolonged effect)
- Any contraindication to general anaesthesia
- Family history of malignant hyperthermia
- Severe burns
- Numerous neuromuscular contraindications including spinal cord injury and dystrophia myotonica
- Pseudocholinesterase deficiency
- Hyperkalaemia / crush injuries
Mechanism
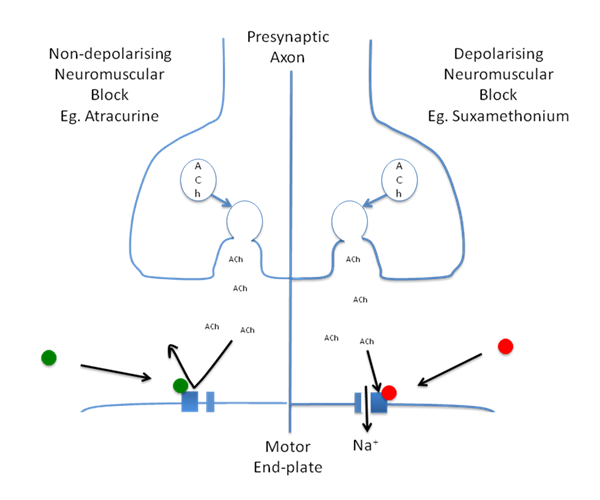
Non-depolarising neuromuscular blocking drugs act as competitive antagonists of the acetycholine channels of the motor end plate. The drugs bind the channel and stop ACh from binding and opening the channel to Na+, preventing action potentials in the muscle fibres. It is necessary to block 70-80% of receptors before transmission fails and paralysis results.
Depolarising neuromuscular blocking drugs act as acetylcholine agonists on the ACh channels of the motor end-plate. Their binding results in the continuous production of action potentials until exhaustion of the cell's ability to repolarise occurs, causing neuromuscular paralysis. The suxamethonium is rapidly broken down by plasma cholinesterase, once this has happened repolarisation again becomes possible and neuromuscular function returns.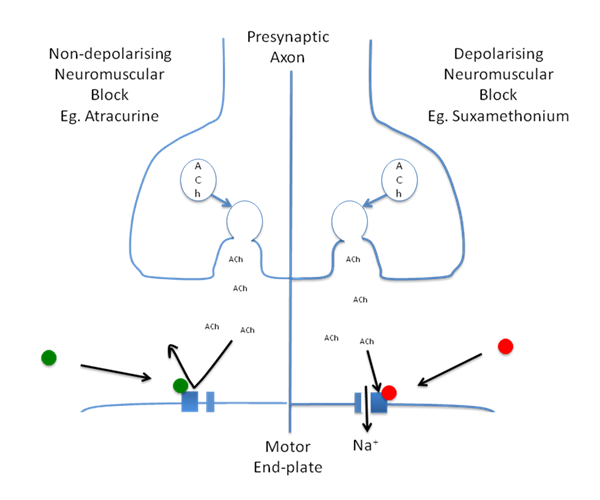
Depolarising neuromuscular blocking drugs act as acetylcholine agonists on the ACh channels of the motor end-plate. Their binding results in the continuous production of action potentials until exhaustion of the cell's ability to repolarise occurs, causing neuromuscular paralysis. The suxamethonium is rapidly broken down by plasma cholinesterase, once this has happened repolarisation again becomes possible and neuromuscular function returns.
Administration
Intravenous
Adverse Reactions
Non-depolarising neuromuscular blocking drugs
- Histamine release (atracurium / mivacurium)
- Allergy
- Hyperkalaemia
- Malignant hyperthermia
- Prolonged paralysis (cholinesterase deficiency)
- Post-operative muscle pains
Interactions
- Inhalational anaesthetics potentiate non-depolarising drugs
- Aminoglycosides, polymixins, clindamycin, colistin, quinine, quinidine and magnesium salts potentiate the action of both depolarising and non-depolarising drugs.
- Drugs that inhibit pseudocholinesterase potentiate the action of suxamethonium (MAOIs, cyclophosphamide, chlorpromazine, trimethoprim, glucocorticoids)
- Cardiac glycoside effects can be potentiated by suxamethonium
Education
Nil of note.
Pharmacokinetics
The non-depolarising agents are metabolised by the liver or excreted unchanged in the urine. The exception is atracurium, which hydrolyses spontaneously in the plasma.
Suxamethonium is broken down by plasma cholinesterases, with about 10% being excreted by the kidneys. Suxamethonium is subject to inter-patient variability depending on the individual's cholinesterase levels and rarely this is so low or absent that there is prolongation of muscle paralysis.
Suxamethonium is broken down by plasma cholinesterases, with about 10% being excreted by the kidneys. Suxamethonium is subject to inter-patient variability depending on the individual's cholinesterase levels and rarely this is so low or absent that there is prolongation of muscle paralysis.
