- Curriculum Overview
-
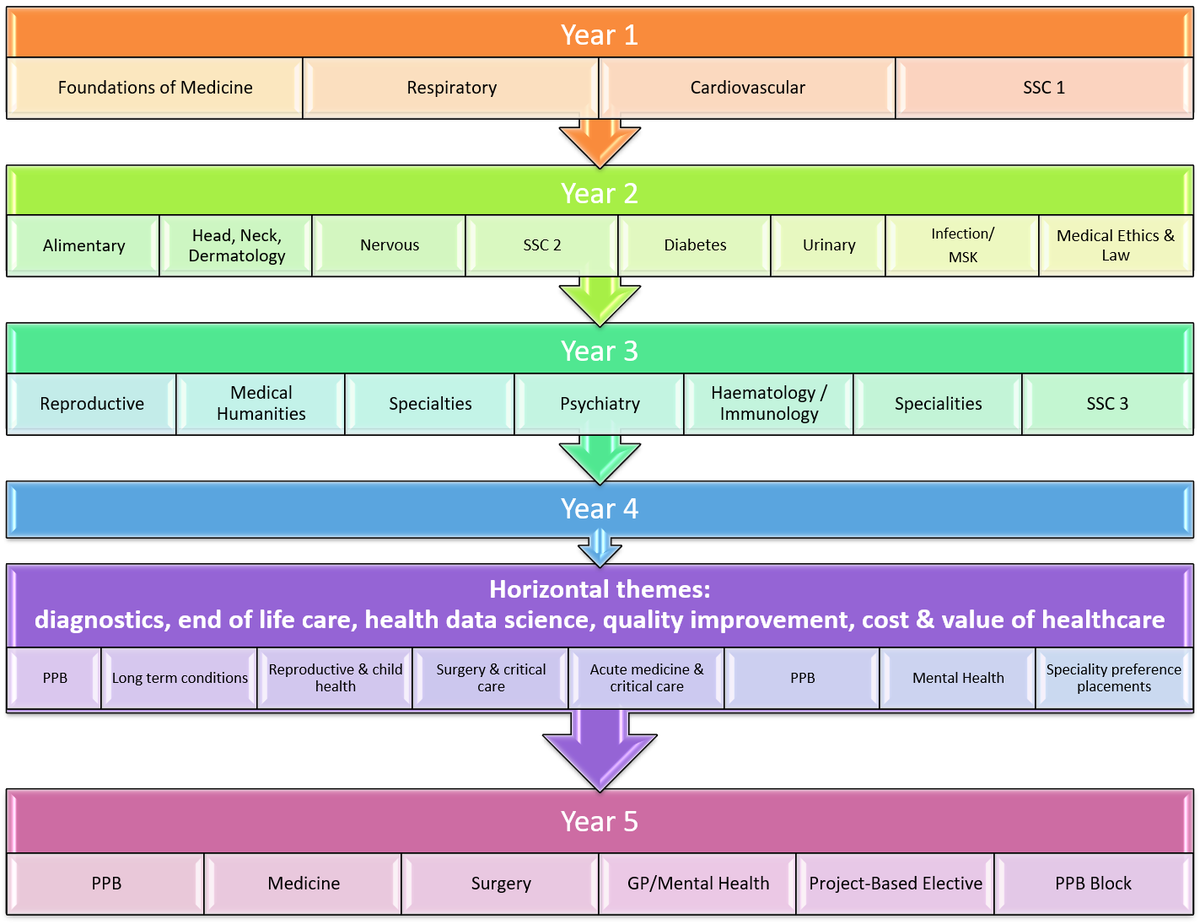
Year 1 In term 1 you will study:
- Foundations of Medicine - principles of normal function of the human body, principles of disease development and management and principles of General Practice.
- Anatomy - introduction to the study of the structure of the human body, including anatomical terminology, commencing with bones and joints, muscles and nerves and the back and spinal cord.
- Clinical Skills - introduction to the practical and communications skills that will form the foundations of your medical practice. Dealing with medical emergencies will also be covered in this first term and revisited throughout the programme.
In Term 2, you start your tour of the body systems with two major systems, the Respiratory System and the Cardiovascular System. These constitute the Medicine 1 course. In this, you will learn about the fundamental structure and function of each system and the clinical application of that knowledge to disease processes. Anatomy 1 and Clinical Skills 1 will continue with a focus now on these systems. You will experience your first clinical attachments in term 2 also.
Through the year a series of clinical cases will be introduced. These will consist of a trigger - usually a clinical scenario with supplementary information - and a series of related questions. The aim of these is to supplement the formal teaching of the curriculum with “real-life” examples to encourage integration of traditional pre-clinical and clinical material, and of material taught in other sections of the MBChB programme.
The GP Enhanced programme at Aberdeen Medical School provides students with innovative experiences and teaching in General Practice and the community. The aim is to ensure all students leave with a good understanding of generalism and what it means to practise as a generalist. In addition to core teaching, there will be additional 'opt in' learning activities available throughout Years 1-5.
Towards the end of term 2 you will engage in the first Student Selected Componen t which gives you an opportunity to work in small groups and study a particular topic in depth.
Year 2 In Term 1, you continue the tour of the major body systems in the Medicine 2 course, beginning with the Alimentary system, Head/Neck/Dermatology and Nervous system. There will be further anatomy and clinical skills teaching and opportunities to practice your clinical skills within each system throughout this year. You will revisit and extend your resuscitation practice. Teaching in General Practice continues, building on the material learned in Year 1. At the start of Term 2, the second Student Selected Component gives an opportunity to choose a particular topic to study in greater depth. The Medicine 2 course resumes after the Student Selected Component, with Diabetes/Endocrine and Urinary Systems.
Late in year 2 students move on to study Advanced Infection, the Musculoskeletal system and Medical Ethics & Law.
Year 3 Year 3 begins with the Reproductive System. This is followed by a 6-week Medical Humanities course which provides an opportunity to select a particular topic to study in greater depth. After this, Specialties and Professional Practice teaching takes place. The Specialties include: Medicine of Old Age, Anaesthetics, Clinical Genetics and Clinical Pharmacology. General Practice teaching continues in this term. In Term 2, Year 3 concludes with Psychiatry, Haematology/ Immunology and Paediatrics teaching.
In Year 3, you will get to experience a wide range of bi-weekly clinical attachments and by the end of the year, you will be able to perform a complete head-to-toe examination of your patients.
The final term in Year 3 will commence with a SSC exploring the wider public health aspects of medicine - Clinical Effectiveness. After a short break, you will start the first of nine five-week clinical rotations that will be undertaken throughout Year 4.
Year 4 Senior Clinical Practice
The Year 4 curriculum is a clinically-based, person-centred learning experience that builds on the breadth and depth of specialty knowledge from the earlier years systems- based teaching. Students develop their clinical reasoning, diagnostic and management skills for both individual patients and patient populations of all ages, with medical conditions affecting any of the body systems. Students undertake seven six-week clinical blocks during which experience will be gained in many different clinical areas and disciplines including:
- Acute medicine and critical care
- Surgery and critical care
- Reproductive and child health
- General Practice
- Long term conditions and integrated care
- Mental Health
- Diagnostics and student preference attachments
At least one of these clinical blocks will be undertaken in Inverness. However, students may choose to undertake the Remote and Rural option for all the blocks in Year 4, and these students will be based in Inverness for the year.
Five horizontal themes also arc across the curriculum: diagnostics, end of life care, health data science, quality improvement, cost and value of healthcare.
Year 5 Professional Practice
Final year represents a deliberate change in approach from the systems-based learning of Years 1 to 4, to experience professional practice as a member of the clinical team dealing with the whole patient.
The year comprises five courses in all. There are three 8-week clinical attachments in the broad areas of Medicine, Surgery and Community Health (General Practice or Psychiatry). As far as possible, students have a choice of specialty within these blocks. Each of these courses covers generic core skills, common to all areas of medical practice, in which students are required to become proficient.
At least one of the clinical courses will be undertaken in Inverness or Elgin. However, much of the time is spent on areas of particular interest to the individual.
Year 5 is very much an apprentice year when students become much more actively involved in the role they will be expected to perform as Foundation Doctors.
Of the remaining two courses in Year 5, one is a project-based Elective on a medical topic. This is an 8-week block which students arrange by themselves, with help from a local supervisor and a network of Electives Advisers.
The other course is the Professional Practice Block which is split into 2 sections, one at the start of the year and the other at the end. This course is designed to facilitate the transition from student to Foundation Doctor and covers practical issues such as dealing with death and dying, ethics and the law, careers, stress in the workplace, time management etc.

[
- Assessment
-
Exams are never a popular feature of any undergraduate curriculum, but the Medical School has a duty to ensure that our graduates have achieved a safe and satisfactory standard of performance in all the elements of medical practice.
Assessment is built in throughout the five years of the course, this helps ensure that basic skills are mastered before moving on to more advanced topics.
Since medicine is not simply a theoretical subject, teaching and learning covers knowledge, skills and attitudes so assessment must therefore do the same.
Medical Licencing Assessment (MLA)
The MLA will set a common threshold for safe medical practice in the UK. If you'll graduate from a UK medical school from the academic year 2024-25 and onwards, you will take the MLA as part of your degree.
More information can be found here
Formative Assessments
Formative assessments are widely distributed within the course and their purpose is to provide feedback to students on how well they are performing.
There is no sanction or penalty for failing these "practice" exams - they are intended to provide an early warning to students that they are not reaching the required standard. There are extensive support mechanisms within the School and formative exams often help staff to identify students who need help for one reason or another, eg because of illness or personal or financial difficulties.
Summative Assessments
Summative assessments are degree exams, usually at the end of a year. These are the "official" assessments that determine whether a student is good enough to proceed to the next year of the course, or to graduate at the end of the course. Students normally have two opportunities to pass such assessments.
A variety of assessment methods are used to carry out formative and summative assessments including:
Written Exams
These test factual knowledge, but can also test clinical reasoning/diagnostic skills and, to a lesser extent, attitudes. The format of written exams includes short answer questions, extended matching questions and single best answer questions.
Course Work
In some courses, essays or reports are written. Some courses also involve students working in groups to produce posters or oral presentations.
Clinical Exams
Clinical skills include history taking, communication skills and examination technique. Diagnostic skills, knowledge of disease management and a wide range of professional skills including ethics are also encompassed within clinical exams. These are tested in the following way:
Objective Structured Clinical Examinations (OSCE)
- OSCEs comprise of a sequence of stations, usually between 12 to 18, each of which tests the candidate on his/her ability to perform a specific clinical task or solve a clinical problem in an allotted time period.
- After Graduation
-
Outcome of the Course
POSTGRADUATE FOUNDATION TRAINING AND BEYOND
At the end of the undergraduate programme you will receive your MBChB degree, which is a primary medical qualification (PMQ). Holding a PMQ entitles you to provisional registration with the General Medical Council, subject only to its acceptance that there are no Fitness to Practise concerns that need consideration. Provisional registration is time limited to a maximum of three years and 30 days (1125 days in total). After this time period your provisional registration will normally expire.
Provisionally registered doctors can only practise in approved Foundation Year 1 posts: the law does not allow provisionally registered doctors to undertake any other type of work. To obtain a Foundation Year 1 post you will need to apply during the final year of your undergraduate programme through the UK Foundation Programme Office selection scheme, which allocates these posts to graduates on a competitive basis. All suitably qualified UK graduates have found a place on the Foundation Year 1 programme, but this cannot be guaranteed, for instance if there were to be an increased number of competitive applications.
Successful completion of the Foundation Year 1 programme is normally achieved within 12 months and is marked by the award of a Certificate of Experience. You will then be eligible to apply for full registration with the General Medical Council. You need full registration with a licence to practise for unsupervised medical practice in the NHS or private practice in the UK.
Although this information is currently correct, students need to be aware that regulations in this area may change from time to time.
There is some discussion about whether to remove provisional registration for newly qualified doctors. If this happens then UK graduates will receive full registration as soon as they have successfully completed an MBChB (or equivalent) degree. It should be noted that it is very likely that UK graduates will still need to apply for a training programme similar to the current Foundation Programme and that places on this programme may not be guaranteed for every UK graduate.
The GMC is currently considering the introduction of a formal assessment that UK medical graduates would need to pass in order to be granted registration with a licence to practise. Although no final decision has been taken as to whether or when such an exam will be introduced applicants should be aware that the GMC envisages that future cohorts of medical students may need to pass parts of a medical licensing assessment before the GMC will grant them registration with a licence to practise.
Postgraduate Foundation Programmes (2 Years)
The Foundation year 1 (F1) enables medical graduates to begin to take supervised responsibility for patient care and consolidate the skills that they have learned at medical school.
The second (or F2) year will allow acquisition of further clinical experience in a broader range of posts allowing, in particular, consolidated development of generic skills. There are a number of criteria which require to be fulfilled and successful completion of FY2 results in the granting of the Foundation Achievement of Competency Document (FACD) which is a requirement for application to Specialty Training.
Foundation programmes will comprise a suite of complementary posts, generally of 4 months duration which will include a number of specialties. Cognisant of our unique opportunities to sample remote and rural aspects of clinical practice, for example in the Northern and Western Isles, many of our Foundation Programmes in the North of Scotland Deanery will include components outwith our main hospital centres.
It is anticipated that Aberdeen graduates will typically continue to undertake their early postgraduate training in the Scottish Foundation School. Applications occur through registration with the UK Foundation Programme Office (a UK wide allocation process). The scheme offers a wide range of programmes, each including a variety of specialties, often in more than one location. You may, of course, choose to work elsewhere in the UK. All UK graduates, no matter their nationality, are entitled under current home office regulations to remain in the UK for the duration of the Foundation Programme.
There are a number of academic programmes available for individuals who wish to pursue an academic career at an early stage. These programmes are advertised and recruited to locally by the relevant Deanery/ Foundation School. Currently, there are academic programmes in the North, South East and West Deaneries in Scotland. This occurs prior to the national recruitment process.
Post-Foundation Training and Career Choice
Foundation Programmes allow a wider taste of different aspects of medical practice than was formerly the case. In addition, taster sessions are available during the programme to try out specialties that you are interested in. This, together with careers sessions within the teaching programme, should help young doctors in choosing a specialty option for subsequent training. The Postgraduate Dean's Staff are always very happy to devote time to doctors who require information about career options for postgraduate training in any branch of medical practice. The Foundation Tutors will play a key role in supporting the doctors at this time and some Foundation Tutors have a specific responsibility for careers.
Specialty Training
The next step in postgraduate medical education, following on from Foundation Programmes, is Specialty Training (ST). There are currently 65 different specialties. General Practice training has also changed and it is now treated the same as other specialties. There have been significant changes in this from the traditional processes. The main difference, is that a doctor applies for training in the speciality of their choice. If successful, a doctor is awarded a National Training Number (NTN) and commences training. On successful completion, the doctor is awarded a Certificate on Completion of Training (CCT). This then allows a doctor to be on the Specialty Register and work as a consultant. The length of time of the training varies from specialty to specialty. In addition, it is competency based so the time served is indicative. In medicine, and only medicine, the doctor will complete a two year "core medical training" and then be allocated to a medical specialty.
Doctors who are unsuccessful in obtaining a Specialty Training post may be able to obtain a Fixed Term Speciality Training Appointment (FTSTA). These are for one year only, do count towards training but do not have a NTN associated with them. Doctors in FTSTA posts will be able to apply to ST posts the following year.
All training is now approved by the Postgraduate Medical Education Board. This includes the training programmes, the approval of the curriculum and the award of the CC.
Academic Medicine
A proportion of graduates with an aptitude for research and teaching follow a career in academic medicine. They will almost invariably proceed on to a degree by thesis eg, MD, ChM or PhD. Individuals who wish to pursue a Consultant appointment in a teaching hospital may also find this form of higher degree invaluable. Potential academics of the future are mentored in Aberdeen and encouraged to apply for the Academic Foundation Programme ( www.abdn.ac.uk/acat ).
For more detailed career information also see: www.nes.scot.nhs.uk .
Planning your Medical Career
The NHS National Medical Careers website www.medicalcareers.nhs.uk contains lots of valuable information to assist you in planning your medical career
International Medical Graduates
UK graduates from overseas who have completed the Foundation Programme and who hope to stay in the UK for further training, may obtain further information from the General Medical Council website.
Medical Councils around the world may have different requirements to practice medicine in their country. Please check with regards to what these may be.
