The four focal countries - Burkina, Benin, Mali and Morocco - were chosen on the basis of facing challenges in maternal heath, having recently
The average rate of skilled attendance at delivery for all developing countries was 42% in 1990, rising to 52% in 2000. However, the average for sub-Saharan Africa was 40% in 1990, rising to just 43% in 2000 (WHO 2006b).
Choice of Focal Countries
- Overview
-
This is reflected in the high maternal mortality situation of the countries included in this study, particularly Burkina Faso, Mali and Benin. Their slow progress is related to the lack of financial and human resources that these countries have. Burkina Faso, Mali and Benin rank 177, 178 and 161 in the Human Development Index (out of a list of 182 countries); Morocco is 130th.
Recent analyses show that they also attract less bilateral and multilateral assistance than Anglophone countries.
Mali and Burkina are amongst the 30 countries contributing to largest amount of ill health worldwide (Ravishankar et al. 2009). However, they rank below 30 with respect to donor assistance for health. Francophone countries appear to have therefore an important unmet need for technical and financial assistance from the international community to improve health including reducing maternal mortality.
WHO has estimated that the maternal mortality ratio in Burkina Faso was 1,000 per 100,000 live births in 2000. While it is worth noting that official estimates are much lower than this (307/100000 for 2008), the authorities have given priority to the reduction of maternal mortality. However, despite efforts to promote antenatal care and improve access to emergency obstetric care, the use of health services remains low (54%, MICS 2006), in part because of growing household poverty and the financial barriers associated with user fees in health facilities. In March 2006, the government made the bold decision of introducing a “subsidy policy” to the cost of delivery and obstetric and neonatal emergency care for women and their babies.
The level of maternal mortality in Benin has reduced from 498 maternal deaths per 100,000 live births in 1996 to 397 maternal deaths per 100 000 live births in 2006 (DHS 1996, DHS 2006). Benin also has some of the highest levels of skilled birth attendance (76% nationwide in 2006) and antenatal care utilisation levels in Africa. However, Benin is not on track to meet its MMR target by 2015. A number of bottlenecks have been identified, in particular related to inequities in the use of skilled birth attendants and access to EmOC, which vary according to wealth quintiles and geographical areas. There are also problems of poor quality of care provided in hospital maternity units which have been documented by several studies (Saizonou et al. 2006; Edson et al. 2007; Stanton et al. 2009).
Health care is prohibitively expensive for the majority of the Malian population, particularly women and children. According to the latest report of the national health accounts (2004), 51 % of health expenditure is supported by households, compared with 22% by the state. Mali has a very high MMR (464/100,000) and low skilled birth attendance (45%) (DHS 2006).
The maternal mortality rate in Morocco is also relatively high (227 maternal deaths/100 000 live births). Low financial accessibility was pointed out as the first barrier to access to care in 74% of pregnant women (PAPFAM 2003-04).
- Burkina Faso
-
Background on the Policy
 The national delivery subsidy policy has 3 parts:
The national delivery subsidy policy has 3 parts:- Subsidies of 80% of uncomplicated deliveries made at the first level of care (i.e. in CSPS and CMAs), 60% of uncomplicated deliveries made at second and third levels of care (CHR and CHU) and 80% of emergency obstetric care at any level. The women pay the remaining percentages
- Transport between facilities is free of charge for all pregnant
- Care is free of charge for indigent pregnant women
Two evaluations of the policy implementation have already been conducted.
The first one was conducted 6 months after the policy introduction by AFRICSanté (formerly GREFSAD), and showed that the implementation had been delayed in several health facilities, and there was no improvement of use of services.
A later evaluation (in February 2009), based on key informant interviews, was more positive but reported 4 main areas of concerns:
(i) absence of clear communication of the content of the policy with women and health staff, which undermined the reproductive rights of women;
(ii) failure to implement free transport between health facilities;
(iii) failure to implement care free of charge for all indigent pregnant women because there were no clear criteria for indigence.
Another evaluation will soon start, also involving AFRICSanté and IRSS, and coordinated by Valéry Ridde (University of Montreal), focussing on policy development and perceptions of women and providers.
Our activities in Burkina will complement this project by focusing on areas which are not investigated by the previous or concurrent projects, including the costs, impact on quality of care and health outcomes, and impact on the local health system.
Country profile
Continent Africa Population (in thousands) 1
15234
Gross national income per capita ($)2
1170
Adult literacy rate (%) 1
28.7
Life expectancy at birth (years) 1
51
Infant mortality rate (per 1,000 live birth) 1
92
Under-5 mortality rate (per 1,000 live birth) 1
169
Maternal mortality ratio (per 100,000 live birth) 1
560
Per capita total expenditure on health (PPP int. $) 1
72
Government expenditure on health as percentage of total health expenditure 1
56.1
Government expenditure on health as percentage of total govt. expenditure 1
13.3
Hospital beds (per 10,000 population) 1
9
Source: 1 WHO: Global Health Observatory; 2 World Bank: Data
- Benin
-
Background on Exemption Policy
 In order to reduce maternal mortality, the Benin government has introduced several new strategies since 2006.
In order to reduce maternal mortality, the Benin government has introduced several new strategies since 2006.The first strategy made kits for obstetric emergencies available to referral hospitals.
The second strategy, which began in 2007, introduced special funds to assist the poorest, including the poorest women who need access to EMOC services (Fonds des Indigents). Social workers in hospital have the responsibility to identify women belonging to this category.
Thirdly, since April 2009, free caesarean sections have been available in 43 private-not-for-profit and public hospitals that provide emergency care. Hospitals are reimbursed 100,000 CFA per woman with a caesarean section to cover laboratory costs (medical check up before medical intervention), drugs, kits, surgery, blood and 7 days hospitalization costs.
Furthermore, the government of Benin is currently testing a results-based financing approach to improve quality of care.
The implementation of the free caesarean section policy has just started and its impact has not been evaluated yet. This project is therefore very timely.
Country Profile
Continent Africa Population (in thousands)1
8,662
Gross national income per capita ($)2
1,510
Adult literacy rate (%)1
40.5
Life expectancy at birth (years)1
57
Infant mortality rate (per 1,000 live birth)1
76
Under-5 mortality rate (per 1,000 live birth)1
121
Maternal mortality ratio (per 100,000 live birth) 1
410
Per capita total expenditure on health (PPP int. $)1
70
Government expenditure on health as percentage of total health expenditure1
51.8
Government expenditure on health as percentage of total govt. expenditure1
10.7
Hospital beds (per 10,000 population)1
5
Source: 1 WHO: Global Health Observatory; 2 World Bank: Data
- Mali
-
Background on Policy
 In order to increase access to this potentially life saving procedure and lower maternal mortality, the government of Mali abolished user charges for caesarean sections in public sector facilities (Centres de Santé de Référence or CSREFs and hospitals) in June 2005. According to the policy, there are now no charges for caesarean-section-related procedures (including hospital stay, drugs, laboratory tests or treatment for complications). In return facilities are provided with kits for 'simple' or 'complicated' caesarean sections and reimbursed on actual costs up to a maximum of US $ 60 (FCFA 30,000) for each caesarean section case.
In order to increase access to this potentially life saving procedure and lower maternal mortality, the government of Mali abolished user charges for caesarean sections in public sector facilities (Centres de Santé de Référence or CSREFs and hospitals) in June 2005. According to the policy, there are now no charges for caesarean-section-related procedures (including hospital stay, drugs, laboratory tests or treatment for complications). In return facilities are provided with kits for 'simple' or 'complicated' caesarean sections and reimbursed on actual costs up to a maximum of US $ 60 (FCFA 30,000) for each caesarean section case.However, user fees are not the only potential barrier to accessing caesarean sections. The available information suggests that important barriers may remain at different levels:
- Community level: Delay or reluctance to deliver in a health facility for financial or cultural reasons. User fees are still charged for normal deliveries and families incur other costs (such as transportation costs) in getting pregnant women to CSCOMs to deliver
- CSCOM/ CSREF level: Although ambulances are stationed at CSREFs to transport women who need to be referred for caesarean sections, resources for fuel and maintenance may not be available
- CSREF level: There are problems of timeliness and adequacy of reimbursements for the costs incurred by CSREFs in providing caesarean section services
Two studies are currently taking place in Mali to study the free caesarean section policy:
- USAID ATN+ santé & Abt Associate. They examine the implications of eliminating user caesarean section charges in the public sector (a) for access to caesarean sections, especially among women from lower socio-economic strata (SES) and (b) for the volume of caesarean sections performed, disaggregated by clinical indications. Finally, this activity seeks to identify the key remaining barriers to accessing caesarean sections for low SES women in order to define appropriate future interventions or programmatic changes to reduce maternal mortality in Mali
- AFD-CRDI; They study the emergence of the policy and the perception of the staff and users
Our project in Mali will complement these two projects by using near miss incidence as health outcome measure and by evaluating the impact on the health system (health services not targeted by the policy)
Country Profile
Continent Africa Population (in thousands)1
12,706
Gross national income per capita ($)2
1,150
Adult literacy rate (%)1
26.2
Life expectancy at birth (years)1
49
Infant mortality rate (per 1,000 live birth)1
102
Under-5 mortality rate (per 1,000 live birth)1
194
Maternal mortality ratio (per 100,000 live birth) 1
830
Per capita total expenditure on health (PPP int. $)1
67
Government expenditure on health as percentage of total health expenditure1
51.4
Government expenditure on health as percentage of total govt. expenditure1
11.8
Hospital beds (per 10,000 population)1
6
Source: 1 WHO: Global Health Observatory; 2 World Bank: Data
- Morocco
-
Background on Policy
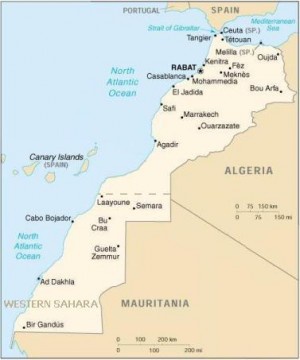
Three actions were prioritised with regards to removal of user fees:
1) Fee exemption for caesarean section and delivery services in the public health care sector;
2) free transportation to public hospitals for emergency obstetric care and
3) improved availability of and free access to medicines, delivery kits and blood transfusion for delivery services in the public health sector.
In 2009, the MOH mobilized an additional budget of about 13 million Euros to implement these decisions. Caesarean section and delivery rates, as well as other process indicators, are monitored to assess the policy implementation, but there is no plan to assess the factors that influence the implementation of this policy and to evaluate the effectiveness and impact of this strategy on the health system and on health outcomes.
This project will appropriately complement the monitoring of the free caesarean section policy in Morocco and will provide a suitable method to evaluate similar policies implemented in the country.
Country Profile
Continent Africa Population (in thousands)1 31,606 Gross national income per capita ($)2 4,190 Adult literacy rate (%)1 55.6 Life expectancy at birth (years)1 72 Infant mortality rate (per 1,000 live birth)1 32 Under-5 mortality rate (per 1,000 live birth)1 36 Maternal mortality ratio (per 100,000 live birth)1 110 Per capita total expenditure on health (PPP int. $)1 202 Government expenditure on health as percentage of total health expenditure1 33.8 Government expenditure on health as percentage of total govt. expenditure1 6.2 Hospital beds (per 10,000 population)1 11 Source: 1 WHO: Global Health Observatory; 2 World Bank: Data
