Insulins
Examples
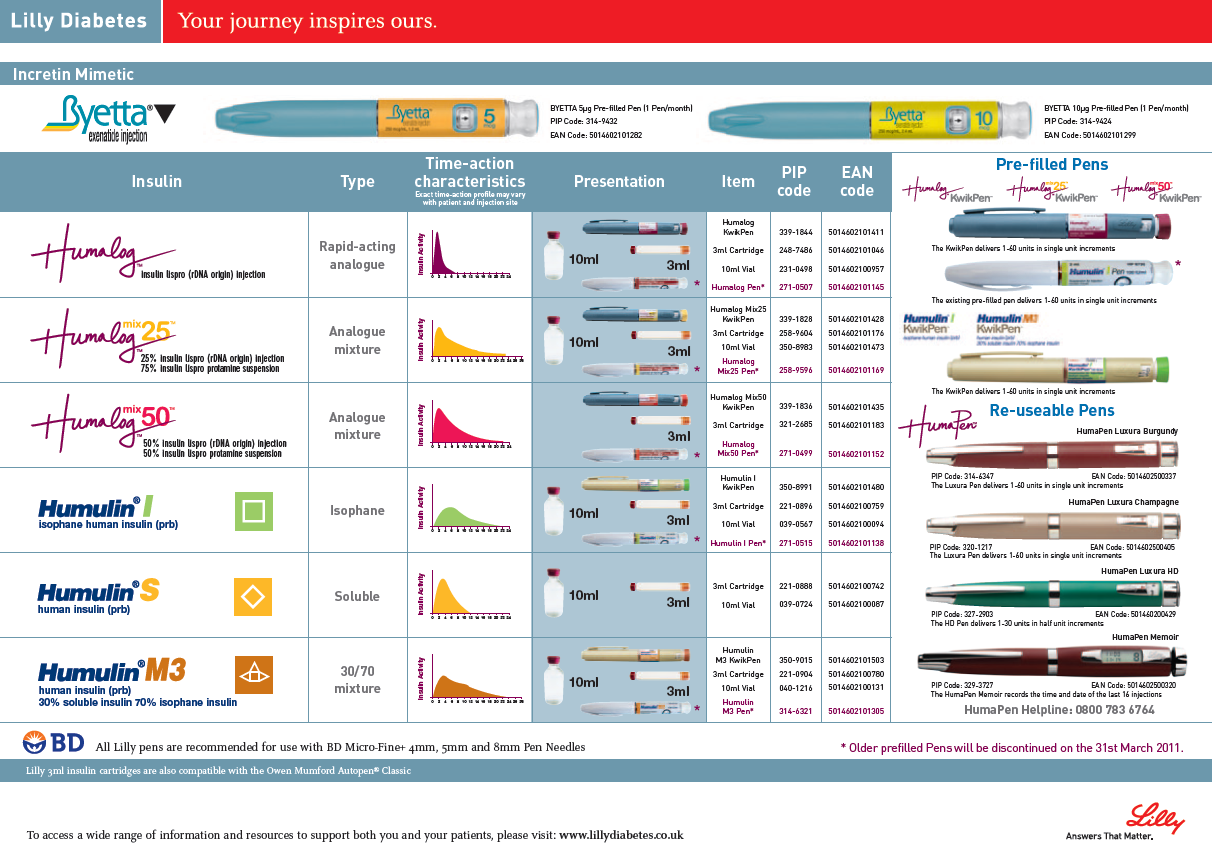
Short acting

- Actrapid (soluble insulin)
- Novorapid (insulin aspart)*
- Humalog (insulin lispro)*
- Novomix 30 (biphasic insulin aspart)*
- Humalog Mix25 (biphasic insulin lispro)*
- Lantus (insulin glargine)*
- Levemir (insulin detemir)*
* = insulin analogues

Indications
- Diabetes mellitus - type 1 or type 2
- Diabetic Ketoacidosis
Contraindications
Caution
- Renal impairment (insulin requirements may be reduced)
- Hepatic impairment (insulin requirements may be reduced)
- Pregnancy and breast feeding (insulin requirements may change - specialist input required)
- Sick days will require insulin adjustment
Mechanism
Insulin is a hormone produced in the pancreatic islet cells. In diabetes, either the production of insulin (type 1) or sensitivity of body tissues to insulin (type 2) is impaired. Insulin is administered to mimic normal production as closely as possible. Different insulin preparations allow prescribers flexibility to do so, with patient needs and lifestyles catered to.
Insulin actions include:
Insulin actions include:
- Increases glucose uptake by insulin-sensitive tissues (e.g. adipose, muscle)
- Increases glycogen synthesis in muscle and liver
- Increases amino acid uptake into muscle
- Increases protein synthesis
- Increases triacylglycerol synthesis in adipocytes and liver i.e. stimulates lipogenesis and inhibits lipolysis
- Inhibits the enzymes of gluconeogenesis in the liver
- Promotes K+ ion entry into cells
Administration
Insulin is a protein and therefore cannot be given orally. The subcutaneous route is most commonly used by patients on a daily basis. Some patients may use a continuous subcutaneous infusion device. Intravenous insulin can be given in hospital. The time to action and half-life of insulin is different between these two routes. Soluble insulin (actrapid) should act within 30 - 60 minutes of subcutaneous injection, with a peak effect between 2 and 4 hours and a total duration of about 8 hours. Given intravenously the time to onset is more like 5 minutes and the effect will last for about 30 minutes. The insulin analogues have faster onset and shorter duration of action.
Commonly used regimens are: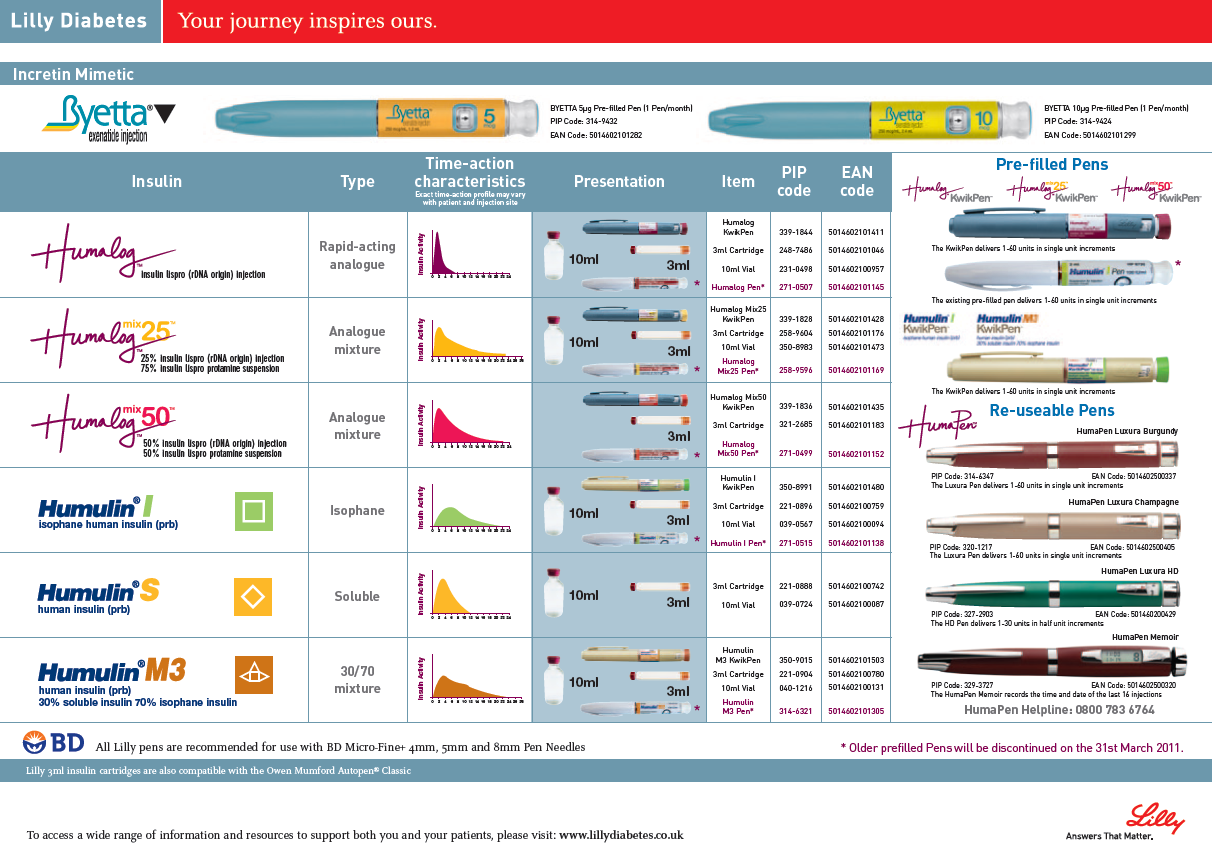
Commonly used regimens are:
- Basal bolus - long acting insulin once a day with short acting insulin before meals
- Twice a day - mix of short and intermediate acting given before breakfast and tea
- Three times a day - mix of short and intermediate acting before breakfast, short acting before tea and intermediate acting at bedtime
Inhaled preparations of insulin have been developed but are still in the research stages.
Adverse Reactions
- Hypoglycaemia is the most common issue with insulin use.
- Various problems such as lipodystrophy, rashes and transient oedema can occur at injection sites, which may be reduced by rotating sites.
Interactions
Pharmacodynamic interactions can occur with medicines which affect blood glucose levels, so any treatment for type 2 diabetes eg gliplizide. In addition, medicines which can reduce glomerular filtration rate may change insulin clearance.
Education
Patient education in diabetes is critical. Refer to lecture notes.
Pharmacokinetics
Each insulin preparation has a slightly different profile which may be useful in patient care. Refer to the manufactures literature.
