Fibrinolytic Drugs (Thrombolytics)
Examples
- Tissue plasminogen activator (tPA) e.g. Alteplase and Tenecteplase
- Streptokinase
Indications
Fibrinolytic agents are used when there is an urgent need to break down a fibrin clot.
- Acute myocardial infarction
- Acute Ischaemic Stroke
- Deep Vein Thrombosis
- Pulmonary Embolism
- Acute arterial thromboembolism
- Central retinal venous or arterial thrombosis
Contraindications
Contraindications:
- Recent or ongoing haemorrhage, trauma, surgery
- Previous intracranial haemorrhage
- Recent ischaemic stroke or head injury
- Known intracranial lesion
- Aortic dissection
- Bacterial Endocarditis
- Acute Pancreatitis
- Recent surgery / invasive diagnostic procedures
- Coagulopathy or anticoagulant therapy
- Prolonged cardiopulmonary resuscitation
- Pregnancy or recent delivery
- Severe liver disease (oesophageal varices)
- Elderly patients
- Severe uncontrolled hypertension
- Proliferative diabetic retinopathy
Mechanism
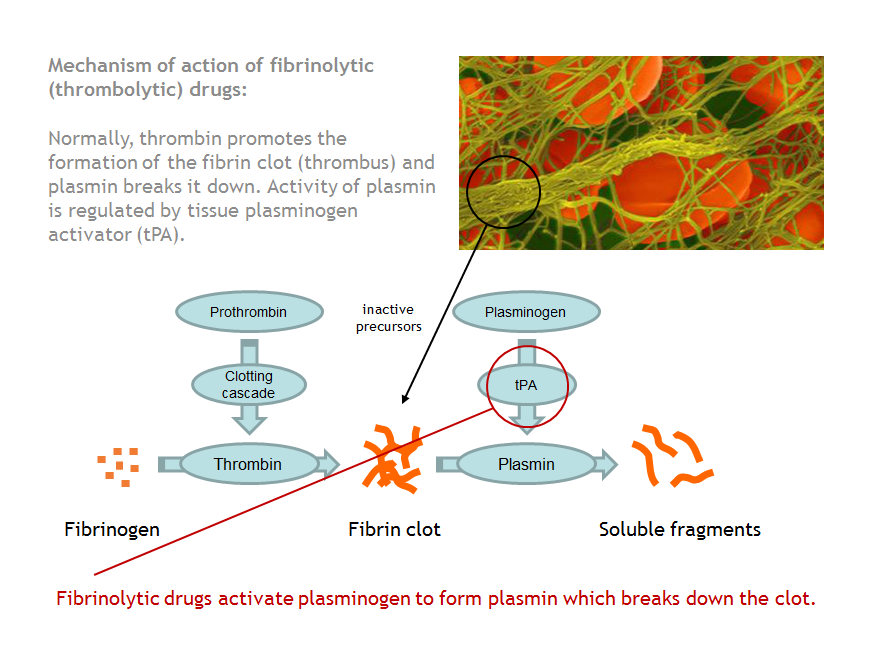
Fibrinolytic agents act in the coagulation pathway, by hydrolysing the peptide bond in the protein plasminogen. The result is activation of the enzyme plasmin which promotes clot lysis.
Administration
IV injection
Adverse Reactions
- Haemorrhage, bleeding is usually only at the injection site, but stroke can occur. Hypertension will increase the risk of haemorrhage occurring. This risk can be reduced in hypertensive patients by administering a nitrate infusion before starting thrombolysis
- Cardiac arrhythmias can develop as a result of myocardium reperfusion. All patients should be closely monitored
- Hypotension (more commonly with streptokinase)
- Nausea / vomiting
- Allergic reaction (streptokinase only)
Interactions
Patients taking warfarin, anti-platelet drugs and corticosteroids are at increased risk of bleeding, however in most circumstances the benefit is likely to outweigh the risks.
Education
Warn the patient about the risks of bleeding, including the risk of stroke.
Pharmacokinetics
Patients who have been treated with streptokinase may form neutralising antibodies to streptokinase. If these patients require thrombolysis again, they should be treated with agent other than streptokinase to avoid an allergic reaction developing.
