Angiotensin Converting Enzyme Inhibitors (ACE-i)
- Ramipril
- Lisinopril
- Enalapril
- Perindopril
- Treatment of hypertension
- MI secondary prevention, especially if there is evidence of ventricular dysfunction
- Treatment of heart failure
- Treatment and prevention of diabetic nephropathy
- Pregnancy - ACE-i have a teratogenic effect
- Bilateral renovascular disease - ACE-i can cause severe renal impairment
- Severe renal failure
- Hepatic insufficiency
- Patients with a fixed cardiac output (e.g. aortic stenosis, mitral stenosis and hypertrophic cardiomyopathy) - ACE-i cause vasodilatation and in these patients a significant fall in blood pressure can occur.
- Breast feeding
- Diabetes (may lower blood glucose)
- Afro-Caribbean patients (respond better to CCBs)
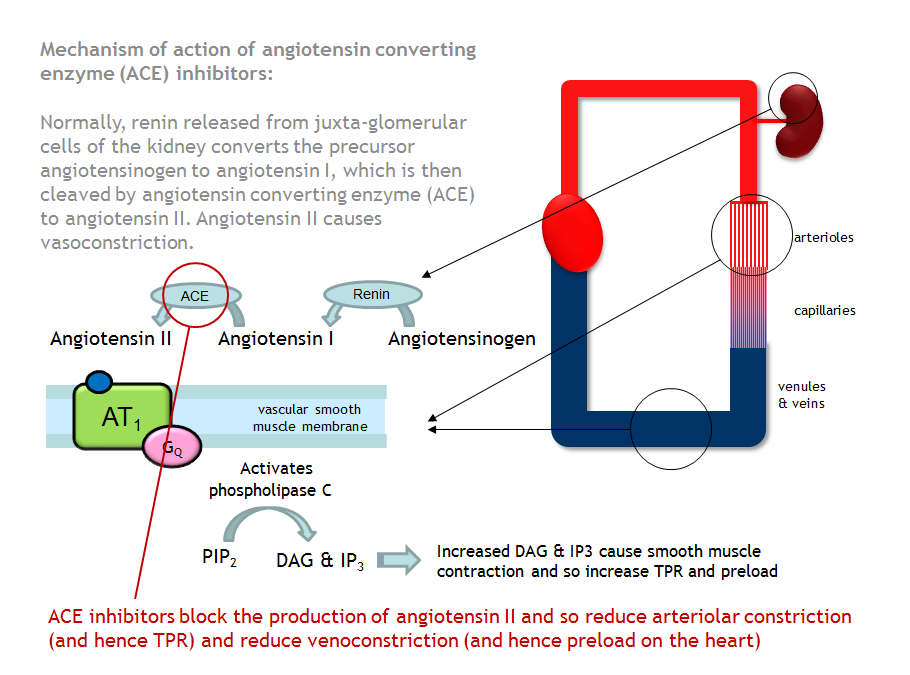
Blood pressure is regulated by the Renin-Angiotensin-Aldosterone system, therfore drugs that act in this system can be used to treat hypertension. Heart failure can be treated by manipulation of this system to change pre-load and after-load on the heart.
Renin is produced by the kidneys in response to renal hypoperfusion. This drives the conversion of Angiotensinogen to Angiotensin I. Angiotensin I is then cleaved by Angiotensin Converting Enzyme (ACE) to form Angiotensin II. Angiotensin II is a powerful circulating vasoconstrictor (acting on the AT1 receptor). It therefore increases peripheral resistance and blood pressure.
ACE inhibitors inhibit one stage of this pathway: the conversion of Angiotensin I to Angiotensin II. This causes a decrease in peripheral resistance, with a reduction in blood pressure (mechanism in hypertension) and a reduction in the end diastolic left ventricle pressure (mechanism in heart failure).
Hypertension: start with low dose and titrate up to blood pressure target. Heart failure: start with low dose and carefully titrate to maximum tolerated dose (hypotension is the most common issue).
Check patient's urea and electrolytes before and 1-2 weeks after starting treatment. This should identify whether the patient's renal function has been impaired and would lead to discontinuation of the drug and further investigation of any kidney pathology.
- Dry cough (occurs in roughly 20% of patients). This is caused by a secondary property of ACE-i's - inhibition of bradykinin metabolism (see diagram).
- Renal impairment.
- First dose hypotension. This is rare but can be problematic in patients on high dose diuretic therapy because of a volume depleted state. It is for this reason that it is recommended that the first dose is taken at bedtime when the patient commences on an ACE inhibitor.
- Hyperkalemia (rare if used as a single therapy). A reduction in Angiotensin II causes a fall in Aldosterone secretion (Aldosterone increases Na+ reabsorption and K+ excretion) leading to a rise in K+.
- High doses can produce a loss of taste.
- Hypersensitivity reactions / angioedema can occur.
- Cholestatic jaundice, hepatitis and hepatic failure.
ACE-inhibitors are strongly contraindicated alongside Angiotensin-II-Receptor-Antagonists. Given together they increase the risk of first dose hypotension, general hypotension and hyperkalaemia.
Loop diuretics and ACE-i can cause hypotension as diuretic therapy will deplete the intravascular volume. In some patients it may be desirable to temporarily stop treatment with diuretics before starting an ACE-i. In other patients, the synergistic effect on blood pressure may be desirable.
ACE inhibitiors are predicted to increase the risk of hypersensitivity and haematological reactions when given with allopurinol.
Inform the patient about the importance of having their blood pressure checked regularly.
If indicated inform the patient about the importance of having their blood tested to assess their renal function and electrolyte status.
