Centrally Acting Anti-Hypertensive Drugs
Examples
- Methyldopa
- Moxonidine
Indications
- Hypertension (specialist use only)
Contraindications
Methyldopa : Contraindications
- Depression
- Porphyria
- Active liver disease
- Phaeochromocytoma
- History of depression
- Renal impairment
- Bradycardia
- Conduction disorders / bradyarrhythmias
- Severe cardiac disease
- Severe liver disease
- Pregnancy and breast feeding
- Renal impairment
- Unstable angina
- Moderate heart failure
- Acute angle glaucoma
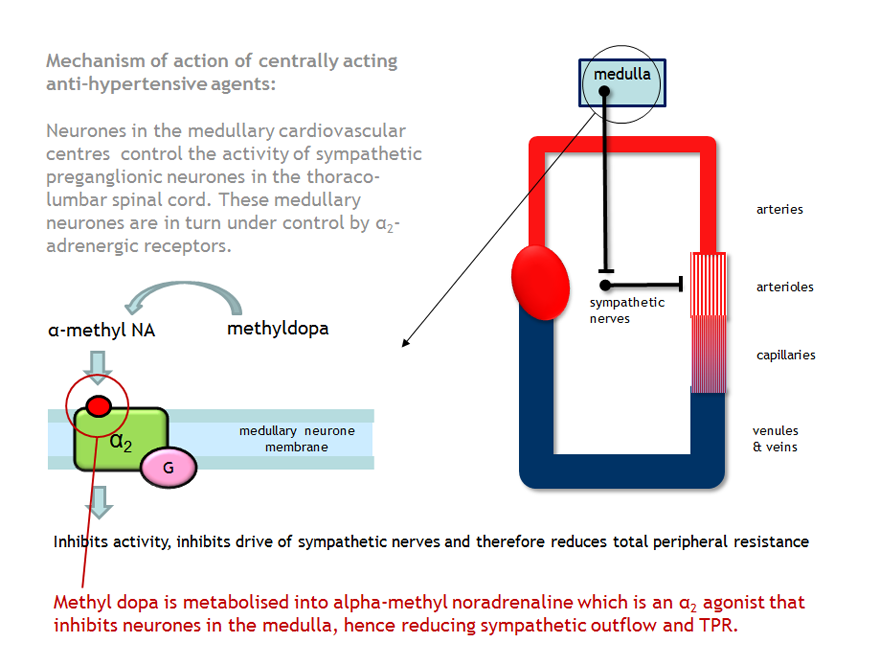
Mechanism
Methyldopa is a centrally acting α2 agonist. At the adrenergic nerve endings methyldopa is metabolised into alpha methyl noradrenaline, an agonist at α2-receptors on pre-synaptic nerve terminals. Stimulation of these receptors results in a reduction in central sympathetic discharge which decreases the systemic vascular resistance and thereby systemic blood pressure. There is minimal effect on cardiac output or heart rate.
Moxonidine is an imidazoline receptor antagonist. It also acts centrally to reduce sympathetic outflow.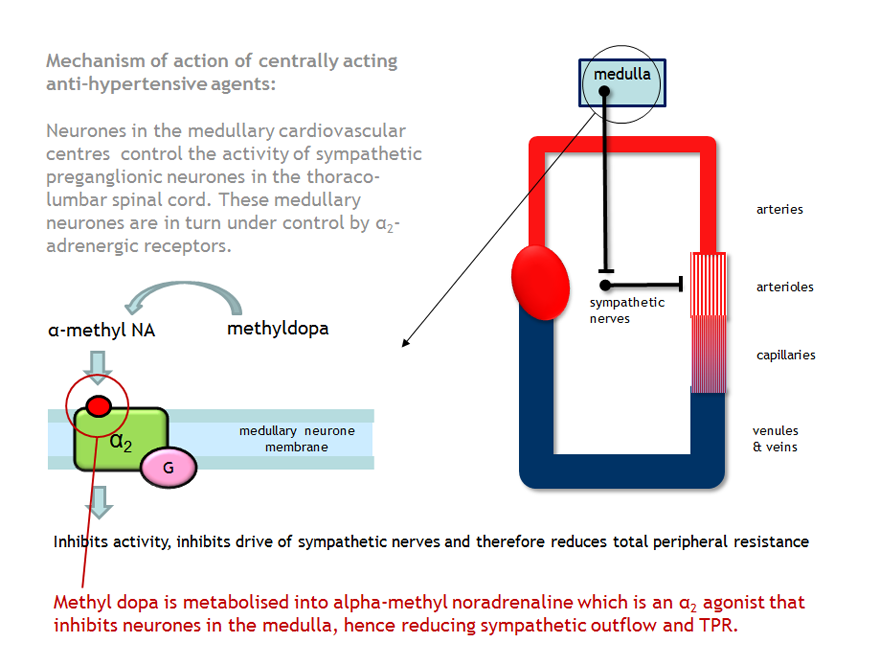
Moxonidine is an imidazoline receptor antagonist. It also acts centrally to reduce sympathetic outflow.
Administration
Oral
Adverse Reactions
Both drugs:
- Sedation
- Lethargy
- Dry mouth
- Postural hypotension
- Positive antiglobulin (Coombs) test is found in 20% of patients
- Haemolytic anaemia (2%)
- Hepatitis
- Lupus like syndrome
- Back pain
- GI upset – nausea, vomiting, diarrhoea, dizziness
Interactions
Methyldopa will increase the neurotoxicity of lithium.
Antidepressants, anaesthetics and salbutamol (via IV infusion) will increase the hypotensive effects of methyldopa.
Moxonidine when combined with some other medications can cause hypotension and CNS depression therefore caution should be exercised when prescribing.
Antidepressants, anaesthetics and salbutamol (via IV infusion) will increase the hypotensive effects of methyldopa.
Moxonidine when combined with some other medications can cause hypotension and CNS depression therefore caution should be exercised when prescribing.
Education
Patients need to be aware of the importance of having their blood tested to assess their FBC and LFT's monitored.
Sedatory effects should be taken into consideration for patients who drive/operate machinery.
Abrupt withdrawal should be avoided.
Sedatory effects should be taken into consideration for patients who drive/operate machinery.
Abrupt withdrawal should be avoided.
Pharmacokinetics
Methyldopa and moxonidine are renally excreted and action may be prolonged in renal impairment.
